ORIGINAL ARTICLE
Brief interventions and tools for nursing care: descriptive and exploratory study
Jacqueline Souza1, Margarita Antonia Villar Luis1, Clarissa Mendonça Corradi-Webster1
1University of São Paulo
ABSTRACT
Aim: to identify the need for brief intervention in a group of male users of a public health service. Method: This is a quantitative study of an exploratory and descriptive nature, whose subjects were recruited through a census. Results: It was found that 67% of the subjects had scores of occasional use, and one of the subjects presented scores indicating dependence. 31% had scores indicating abuse, suggesting, therefore, the possibility of a benefit of brief interventions. Discussion: The study subjects had low education levels and low incomes, two situations that can lead to social vulnerability. Of the subjects who presented scores indicating abusive use, some reported this pattern of consumption for two substances. Conclusion: From these results we highlight the relevance of the integration of brief interventions and evaluative tools related to substance dependence in nursing practice in different health services.
Keywords: Nursing, Mental Health, Substance-related Disorders.
INTRODUCTION
The measures of early detection and prevention of the problems arising from the use of substances optimizes expenditure in the health sector and enables the planning of interventions in the early stages of problems. These factors are directly related to the prognosis in the health and quality of life of the population(1,2).
Thus, there has been an increasing number of investigations related to the development of detection instruments that are valid, reliable and have a low cost for the screening of the issues related to the use, abuse and dependence on alcohol and/or other drugs(3-5).
The term screening refers to the application of a test to estimate, among people, the probability of having a specific disorder, different from a diagnosis with regard to identifying and confirming such disorder. This concept has assumed significance due to the success of preventive actions that occurred as a result of the early detection of diseases such as hypertension, diabetes, cervical cancer and phenylketonuria(5). Moreover, this strategy has been useful in screenings to support interventions in the context of drugs.
The Strategies for Diagnosis and Brief Interventions (BDIS) consists of early recognition and rapid intervention for drug-related problems, and aims to recognize and attend to different patterns of drug use among subjects and assist them in decision-making and efforts to reduce or stop drinking, improve their health and prevent future problems(6).
Brief interventions (BIs) can be used as health education for people who do not use drugs or are at low risk of use, as it can reduce excessive consumption and increase the number of people who seek treatment in the case of substance dependence.
The BI is based on a motivational interview and is performed through brief counseling to help the patient explore and resolve their ambivalence about their use of the substance and unleash the decision and commitment to change their behavior(7).
The level of primary health care (PHC) has been described as the main locus for the implementation of BDIS since medical professionals, nurses, social workers or community health workers take on a strategic position in the management and linking of the subjects of the community. This environment facilitates the identification and referral of people in the early stages of alcohol dependence in order to prevent an increase in dependency. In addition, PHC is critical for identifying risk users who may or may not have developed dependence, but still need to reduce the risk of damage due to alcohol consumption(6-8).
The present study sought to identify the pattern of drug use, to distinguish the different needs of brief intervention in a group of male users of a public health service, and show the potential of the Brief Interventions Strategy as a resource to be used by nurses in the prevention and care of drug use.
METHOD
This is a quantitative study of an exploratory and descriptive nature, whose subjects were recruited from a census. The sample included men who were in the waiting room for care in a medical clinic and the emergency room of a public health center in the municipality of Ribeirão Preto/SP - Brazil during the period of data collection (one week in the month of April 2009), and who agreed to participate in the study, totaling 51 subjects. The ethical precepts were observed and met and the project was approved by the Ethics Committee of the School of Nursing of Ribeirão Preto/SP (protocol 171/2008).
The exclusion criterion adopted was the existence of some important cognitive impairment that would hinder the participation in the study or compromise the reliability of the responses. To identify this criterion the Mini Mental State Examination (MMSE) was used, which is an important screening tool for cognitive impairment for clinical use and research. It is described as one of the most used tools in the world, and the version for the Brazilian population is already validated and was translated by Bertolucci and collaborators(9,10).
The total score can range from 0 to 30 points, where 0 indicates the highest degree of cognitive impairment of individuals and 30 is the best cognitive ability. It takes around five to ten minutes to complete the MMSE and its application can be made both by professionals and by properly trained lay persons(9,10).
We emphasise the need for adjustment of the scores according to the level of education of the individual in order to avoid losses and/or false positives. The cutoffs suggested from validation studies for the Brazilian version were as follows(9-11):
- Illiterate 19 points
- 1-3 years of schooling 23 points
- 4-7 years of schooling 24 points
- More than 7 years of schooling 28 points
In this case, a score equal or greater than the cutoff corresponds to normal cognitive function, and when below the cutoff point there probably is a cognitive deficit(12).
The other instruments used were a socio-demographic questionnaire and an "Alcohol and Substance Involvement Screening Test" (ASSIST). The first was used in order to gather information corresponding to the main individual attributes of the members. The questions were in the format of a questionnaire, based on the minimum social indicators described by the Brazilian Institute of Geography and Statistics(13), covering aspects relating to education and living conditions, family, color or race and work and income.
On the other hand, the ASSIST, developed by a group of researchers in the field of alcohol and drugs from various countries, under the coordination of the World Health Organization (WHO)(2,14), was used to track drug use, frequency of use, feelings of compulsion and other related problems.
The development of the ASSIST was proposed by the WHO in 1997 and the project was conducted in two phases. In phase 1 (1997-1998) a preliminary questionnaire with 12 items was made and the analysis of test-retest reliability was performed involving the following countries: Australia, Brazil, India, Ireland, Israel, the Palestinian Territories, Puerto Rico, United Kingdom and Zimbabwe. The idea of involving different cultures was designed to accommodate the varying usage patterns(2,14).
Then, a review of the preliminary questionnaire was carried out and the new version consisted of eight items that were chosen based on the feedback from the study participants, taking into consideration their ease of application and understandability. Phase 2 (2000-2002) consisted of an international validation study involving Australia, Brazil, India, Thailand, UK, USA and Zimbabwe(2,14).
Therefore, the ASSIST has already gone through the process of translation, performance assessment (concurrent validity and internal consistency), reliability tests (test-retest) and feasibility for use in Brazil. It has a standardised structure, can be rapidly applied, covers various types of substances, and is easy to interpret(14).
The instrument consists of a structured questionnaire with eight questions regarding the use of the following psychoactive substances: tobacco, alcohol, marijuana, cocaine, stimulants, sedatives, inhalants, hallucinogens and opiates. Its goal is to identify individuals using psychoactive substances and to determine the frequency of use (in the last three months and in their lifetime); the use of injectable drugs; feelings of compulsion and other related problems such as impairment in the performance of tasks; concern of others regarding the individual’s use; and attempts to reduce or cease use that were unsuccessful(14). The time needed for its application is about 5 to 10 minutes(2,14).
Each response corresponds to a score ranging from 0 to 4, and the total may vary from 0 to 20. A score of 0 to 3 is considered to be indicative of occasional use, 4 to 15 as indicative of abuse and greater than or equal to 16 as suggestive of dependence (14:200).
| |
The ASSIST demonstrated good discrimination among the low, moderate and high risk usages: it has shown good discriminant validity, especially for alcohol, marijuana, amphetamines, opioids and cocaine. Therefore, it is a useful screening tool for the abusive use of alcohol or other drugs since it allows accurate information to be obtained about the use of different substances and the risk associated with them, showing good construct validity, concurrent validity and discriminant validity(2, 14). |
Furthermore, the time required for its total application is short, a factor that optimises the search process. The prominent features of ASSIST are(2,14): it is relatively brief; it includes ten substances (tobacco, alcohol, marijuana, cocaine, amphetamines, inhalants, sedatives, hallucinogens, opioids and other drugs); and investigates both use frequency and the related problems.
All instruments were filled out by the researchers.
RESULTS
The study subjects were on average 41 years old and had seven years of study. 51% of the interviewees were married, 66% were working at the time of the survey, and of these, 65% earned the minimum wage. The cutoff point for minimum education on the MMSE was 19; the average found among respondents was 27.85, and the minimum and maximum scores were 21 and 30, respectively.
Table 1 shows the drugs that subjects reporting having tried and those they said they consume daily.
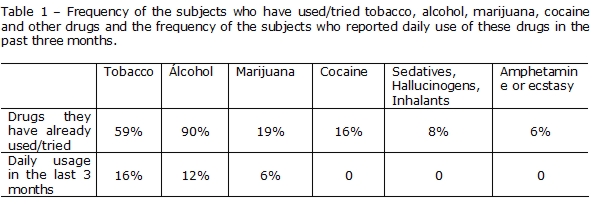
As it can be observed in Table 1, 34% of the interviewees have reported daily consumption of some drug (tobacco, alcohol, marijuana or cocaine). Furthermore, 14% of subjects reported that a family member, friend or colleague has already demonstrated concern about substance use. 14% had already made an attempt to control, reduce or stop using it and failed.
Regarding the pattern of use, we found that 67% of the interviewees had scores indicative of occasional use for some kind of drug, including 29 subjects who occasionally use alcohol, two subjects who use marijuana, one who uses cocaine, another who uses inhalants, and another subject who occasionally uses ecstasy or amphetamine. One of the respondents presented scores indicating dependence on alcohol and cocaine.
Additionally, 31% of the subjects presented scores indicating abusive use of some type of drug (eight subjects with scores of abusive use regarding tobacco, four for alcohol, three for marijuana, and one for cocaine). Of the individuals with scores suggesting abusive use, five presented at-risk consumption for more than one substance, namely: marijuana and tobacco (n=1), tobacco and alcohol (n=2), alcohol and marijuana (n=1) , and marijuana and cocaine/crack (n=1).
DISCUSSION
The results point to the existence of social determinants of health relevance, namely low education, low income and a significant number of unemployed individuals (34%). These three characteristics mark out the social vulnerability of this group.
These conditions of social and material deprivation contribute to the deterioration of health, premature death, risk behavior, and substance use: the worse the condition of life, the greater the potential risks to health are. Therefore, the social determinants of health are one of the main aspects related to substance use(15).
We add that, although drug use occurs in all social layers, the morbidity and mortality related to this behavior are disproportionately higher among the groups with a lower socio-economic status(16).
Therefore, this issue takes on even greater importance in services of a public nature, which are usually the services that attend to more individuals in a situation of social vulnerability. The need for public policies to help this situation, and structural projects aimed at improving income distribution, are paramount as extreme poverty affects health and, above all, the citizenship of these people. In relation to substance use throughout life and everyday use in the last three months, the results of this study showed values above the average found in the last national survey on drug use(17). It has shown that 22.8% had used some drug (that was not alcohol or tobacco) throughout life. The prevalence of alcohol dependence was estimated at 12.3%, whereas the use of alcohol in the 108 largest cities of the country was 74.6%. The most used illegal drug according to the survey was marijuana (8.8%), confirming the results of this study that has also shown marijuana as the most used illegal drug among the respondents (19% reported having used marijuana).
The high percentage of alcohol use (90% reported having used alcohol) can be partially justified since alcohol is a drug of low cost and extremely accessible given its distribution, which is reflected in its spread through all layers of the population. In addition, the television media, which also affects a large section of society, widely spreads advertisements associating its consumption with pleasure, leisure and wellness.
Given that 14% of the respondents reported that some member of their social network has already mentioned concerns about their substance use, we must highlight the role of family, relatives and friends in both the perception of the diagnosis and the incentive to search for treatment. Health professionals also have great relevance, especially in identifying substance users among the population assisted by other clinical demands, such as chronic illnesses or emergencies (the subject of this study), as well as in the implementation of interventions related to drug use.
One particular study(18) showed that an individual's perception of their own consumption pattern, or even the receipt of information about their probable dependence, may become a motivational factor to search for formal treatment.
In relation to unsuccessful attempts to change the pattern of substance use reported by the respondents, as well as the high rate of scores indicating abuse, in some instances for more than one substance, there is growing demand for formal treatments(19). Formal support is provided by people who are formally qualified and trained to provide assistance, such as psychologists, social workers and other professionals.
The different treatment modalities can be described as specific sources of formal support and public services. Other private and diversified forms allow the assistance to meet the needs of the different personalities and social functioning of individuals who are substance dependents. However, a signal regarding the need for treatment needs to be provided mainly by a health professional, who must be instructed with knowledge and appropriate skills to approach and motivate patients. It is worth mentioning that the subject who presented a high risk score was instructed regarding his probable dependence and the treatment options in his territory.
In this sense, we highlight the role of the nurse who, during his nursing consultation, may include the use of screening tools, as well as brief intervention, to address these issues (20).
CONCLUSION
The individuals interviewed have low schooling and income, two situations considered to make a person socially vulnerable. Most subjects presented low-risk consumption. However, a large number of individuals presented with scores indicative of abuse, and some of them showed this consumption pattern for two substances. ASSIST proved to be a user-friendly and useful instrument in tracking the use of different psychoactive substances. Based on these results, we highlight the relevance of the insertion of the themes of "brief interventions" and assessment tools and substance use screening into nursing curricula, in the context of mental health, in order to equip future nurses with preventive and interventional tools related to the use, abuse and dependence on substances. It is also recommended that these strategies and tools are used in different health services.
We may highlight, as limitations of the study, the sample size and how the subjects were selected, preventing generalization and the use of statistical tests, which are factors that limited the description of the results. A randomized sample would provide more reliable results. As the implementation of the instruments was well accepted among the subjects, a future potential study could allow the identification of the feasibility of this approach, considering the application time and enabling the discussion of important issues related to substance use by health service users and its importance in nursing practice.
REFERENCES
1. Formigoni ML (coordenadora). A intervenção breve na dependência de drogas: a experiência brasileira. São Paulo: Contexto; 1992.
2. Who Assist Working Group. The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility. Addiction. 2002; 97(9):1183-94.
3. Gorenstein C, Andrade LHSG, Zuardi AW. Escalas de Avaliação Clínica em Psiquiatria e Farmacologia. São Paulo: Lemos; 2000.
4. Ronzani TM, Ribeiro MS, Amaral MB, Formigoni MLOS. Implementação de rotinas de rastreamento do uso de risco de álcool e de uma intervenção breve na atenção primária à saúde: dificuldades a serem superadas. Cad Saúde Pública. 2005; 21(3):852-61.
5. Fleming MF. Screening and Brief Intervention in Primary Care Settings. Alcohol Res Health. 2004; 28(2):57-62.
6. Minto EC, Corradi-Webster CM, Gorayeb R, Laprega MR, Furtado EF. Intervenções breves para o uso abusivo de álcool em atenção primária. Epidemiol Serv de Saúde. 2007; 16(3): 207-20.
7. Segatto ML, Pinsky I, Laranjeira R, Rezende FF, Vilela TR. Triagem e intervençãio breve em pacientes alcoolizados atendidos na emergência: perspectivas e desafios. Cad Saúde Púb. 2007; 23(8):1753-762.
8. Marques ACPR, Furtado EF. Intervenções breves para problemas relacionados ao álcool. Rev Bras Psiquiatr. 2004; 26 (Supl I):28-32.
9. Almeida OP. Mini Exame do Estado Mental e o Diagnóstico de Demência no Brasil. Arq Neuro-Psiquiat. 1998; 56(3):605-12.
10. Chaves MLF. Testes de avaliação cognitiva: Mini-Exame do Estado Mental, 2006-2008 [ article on the internet ]. Cited 2008 Jan 15. Available from: www.cadastro.abneuro.org/site/arquivos_cont/8.pdf.
11. Brucki SMD, Nitrini R, Caramelli P, Bertolucci PHF, Okamoto IH. Sugestões para o uso do Mini-Exame do Estado Mental no Brasil. Arq Neuropsiq. 2003; 61(3):777-81.
12. Ferrari JF, Dalacorte RR. Uso da Escala de Depressão Geriátrica de Yesavage para avaliar a prevalência de depressão em idosos hospitalizados. Scientia Medica. 2007; 17(1):3-8.
13. IBGE [ homepage on the internet ]. Síntese de Indicadores Sociais 2002 [ Cited 2007 Jn 18 ]. Available from: http://www.ibge.gov.br/home/estatistica/populacao/condicaodevida/indicadoresminimos/sintesedeindicsociais2002.shtm.
14. Henrique IFS, Micheli D, Lacerda RB, Lacerda LA, Lacerda LA, Formigoni MLOS. Validação da versão brasileira do teste de triagem do envolvimento com álcool, cigarro e outras substâncias (ASSIST). Rev Assoc Med Bras. 2004; 50(2):199-206.
15. Baumann M, Spitz E, Guillemin F, Ravaud JF, Choquet M, Falissard B. Associations of social and material deprivation with tobacco, alcohol, and psychotropic drug use, and gender: a population-based study. Intern J Health Geogr. 2007; 6(1):50.
16. Galea S, Vlahov D. Social Determinants and the Health of Drug Users: Socioeconomic Status, Homelessness, and Incarceration. Public Health Rep. 2002; 117(Suppl 1):S135-45.
17. Carlini EA (supervisão). II Levantamento Domiciliar sobre o uso de drogas psicotrópicas no Brasil 2005: estudos envolvendo as 108 maiores cidades do país. São Paulo: CEBRID; 2006.
18. Fontanella BJB, Mello GA, Demarzo MMP, Turato ER. Percepção da síndrome de dependência por pacientes em tratamento. J Bras Psiq. 2008; 57(3):196-202.
19. Barker C, Pistrang N. Psychotherapy and social support Integrating research on psychological helping. Clin Psychol Rev. 2002; 22(3):361–79.
20. Gonçalves SSPM, Tavares CMM. The community-based health nursing to drug abuse. Online Braz J Nurs [ serial on the internet ]. 2005 August [ cited 2011 Aug 10 ] ; 4(2) Available from: www.uff.br/nepae/objn402goncalvesetal.htm
Received: 11/11/2011
Approved: 23/01/2013
Authors
Jacqueline de Souza - Author and executor of the research project.
Margarita Antonia Villar Luis - Research project advisor.
Clarissa Mendonça Corradi-Webster - Active researcher in the data analysis and article revision stages.